- Site-by-site vaccinations at the places of residence and other locations previously visited by cases
- Simultaneous vaccination of healthcare and frontline workers (HCW/FLW) and others at increased risk working in healthcare facilities
- Pop-up vaccination, where those at risk are invited to an agreed upon location outside their place of residence
- Targeted geographic vaccination of villages if contacts, and contacts of contacts, cannot be clearly ascertained due to security constraints, but are invited to a previously agreed upon site to be vaccinated
Continued Spread
Despite the availability of a vaccine and the vaccination of approximately 150,000 people in the DRC as of July 6, 2019, new cases and hot spot areas continue to pop up. The outbreak seems to be escalating rapidly – although it took eight months to reach 1,000 reported cases, it took only 71 days to double that number.
Confirmed on June 11 in the Kasese District, near the border with the DRC, the first case of Ebola in Uganda was a five-year-old boy who returned from the DRC with his family after attending the funeral of a family member who had died from Ebola. Since then, two Ebola-related deaths have been reported, including the boy’s, and Uganda has initiated a response plan and allocated supporting budget.
On July 17, 2019, at the fourth meeting of its International Health Regulations Emergency Committee since the outbreak was declared, the WHO declared the outbreak in the DRC a Public Health Emergency of International Concern (PHEIC). This follows recent activity in the country, including the first case to be confirmed in Goma, a large city on the border with Rwanda.
WHO Director-General Dr. Tedros Adhanom Ghebreyesus stated, “It is time for the world to take notice and redouble our efforts. We need to work together in solidarity with the DRC to end this outbreak and build a better health system. Extraordinary work has been done for almost a year under the most difficult circumstances. We all owe it to these responders — coming from not just WHO but also government, partners and communities — to shoulder more of the burden.”
Despite the rapid response and vaccination effectiveness, new cases are continuing to occur. Effective, widespread, and coordinated public health efforts in countries such as the DRC are often challenged by limited healthcare resources, other disease outbreaks, violence, deteriorating security, general distrust of foreigners and the government, and a lack of funding.
Healthcare resources
DRC has the third lowest GDP in the world, and there are only 0.09 physicians/1,000 population (compared with 2.59 physicians/1,000 population in the US). Hospitals and clinics lack personnel and equipment and often run out of critical medicine and supplies. In the current Ebola outbreak, healthcare resources are further stretched by fatigue among the response staff and ongoing strain on limited resources, including the increasing number of cases among health workers (6% of total cases).
Other disease outbreaks
The European Commission Emergency Response Coordination Centre (ERCC) reported on June 13, 2019 that 12,000 cholera cases had been reported in 20 of 26 provinces (including North Kivu) since the beginning of 2019, including 260 deaths. A cholera vaccination campaign was started by the Congolese Ministry of Health at the end of May for more than 800,000 people in North Kivu, and approximately 350,000 people had been vaccinated as of June 1, supported by the WHO and The Vaccine Alliance GAVI.
At the same time, an ongoing measles outbreak has affected nearly 100,000 people in 23 of the 26 DRC provinces so far this year, resulting in 1,562 deaths to date, and more than 7.6 million cases of malaria have been reported, including 7,652 reported deaths (as of June 13).
Violence and insecurity
DRC, particularly in the eastern area of the country, continues to be an area of conflict, with more than 100 armed groups active in the region. Ongoing conflict has displaced parts of the population to other areas of the DRC as well as into neighboring countries. These security issues have increased the transmission of Ebola to previously unaffected areas and have made it challenging to identify new cases, trace contacts of confirmed cases, and perform community outreach.
In addition, health facilities have been attacked. Between January and mid-May, 130 attacks on health facilities resulted in four deaths, injuries to an additional 38 people, and a new spike in Ebola cases. In February of this year, a Doctors Without Borders/Médecins Sans Frontières (MSF)-managed Ebola Treatment Center (ETC) in Katwa was attacked and partially burned down, forcing the site to cease operating. Three days later, another joint MSF/Ministry of Health-managed ETC and its vehicles were attacked, with fire destroying the facility. Because these facilities also provided supportive care, such as proper hydration, as well as treatment for malaria and other co-infections, these attacks have seriously hampered public health efforts.
Four Points of Control (PoCs) were involved in security incidents carried out by unidentified armed people earlier this month, interrupting activities throughout the day.
By suspending or delaying case investigation and response activities, attacks and insecurity have hampered intervention effectiveness.
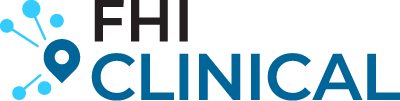
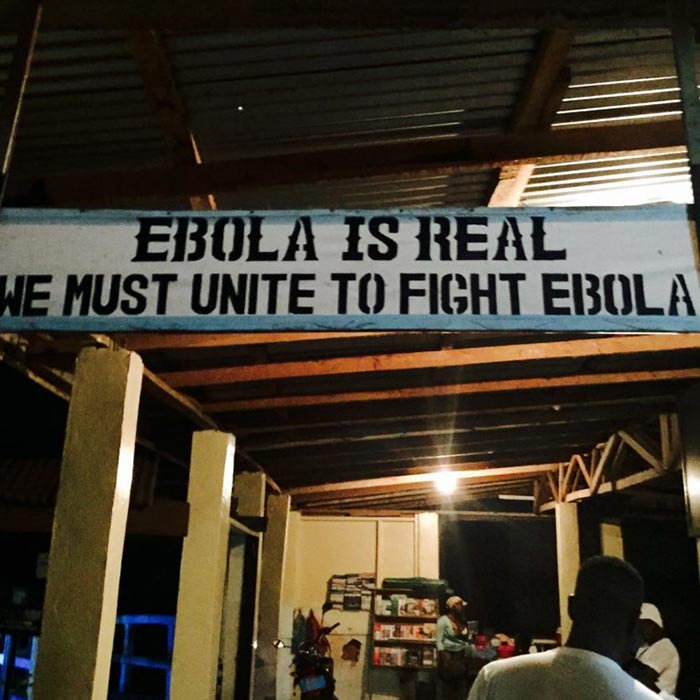
General distrust of foreigners and the government
Given the decades of corrupt government, misrule, and tumultuous political environment, it is not surprising that pockets of mistrust exist toward government-led initiatives and outsiders. But, this often means that people hide sick relatives, bury their deceased family members in secret, and are reluctant to consent to treatment or vaccination. The WHO reported that a lack of community consent meant it was not possible to define rings around 175 (18%) of the cases of Ebola virus disease that had occurred as of March 25, 2019.
Funding
According to the WHO, an additional $54 million USD is needed to fill the funding gap to carry on response activities. WHO Member States have been strongly encouraged to provide donations amid fears that the outbreak will be prolonged without the required resources.
Where to From Here?
It is promising that no new cases or deaths have been reported in Uganda, partly because of its rapid response to the confirmed cases, which included proactive vaccination of HCW/FLWs and isolation of contacts – vaccinating 1,507 consenting individuals (74 contacts, 747 contacts of contacts, and 682 FHWs).
Reports from the WHO indicate that some of the security challenges are being addressed, and community acceptance and case investigations have improved following recent community dialogue, outreach initiatives, and restored access. The declaration of the situation as a PHEIC will ensure that there is a coordinated international response. As a level 3 emergency (the most serious), the outbreak will receive the WHO’s highest level of support. The United Nations has also activated the Humanitarian System-wide Scale-up to address the situation.
The WHO has been collecting data about the vaccine’s effectiveness, which provides evidence of the role of ring vaccination for Ebola, when combined with other key control measures, and of the importance of continuing the vaccination efforts of contacts, contacts of contacts, and FLW/HCWs.
The current situation has also highlighted how important it is to partner with experienced organizations that are able to quickly and effectively strategize to overcome the challenges at hand. Even MSF has indicated that this is the first time that they have tried to address an Ebola outbreak in the midst of conflict, and that they were unprepared.
With our history of managing clinical research in resource-limited settings, our project team quickly deployed high-quality interventions and study support for the Sierra Leone Trial to Introduce a Vaccine Against Ebola (STRIVE) study. As a result, the first vaccination site was opened and enrolled the first patient just over six weeks after our start-up team arrived in Sierra Leone.