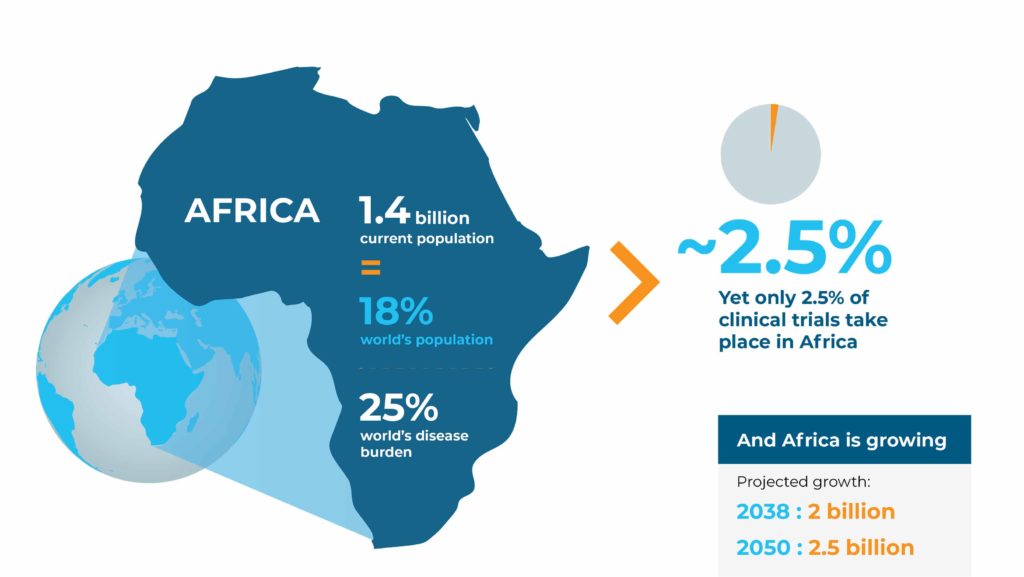
Representing only 18% of the world’s population,1 the continent of Africa carries an inordinate 25% of global disease burden. With a growing population and increasing rates of communicable and non-communicable diseases alike, incongruously, only 2.5% of all clinical trials worldwide are being conducted in Africa.
At FHI Clinical, we see this as a missed opportunity to not only use clinical trials to deliver and tailor medicines and vaccines to populations who need them but also refine efficacy and safety assessments by including treatment-naive, diverse populations. The continent of Africa offers unique ways to identify and develop new therapies owing to its diverse population, pathogenic profile, environment and disease epidemiology.
A diverse continent
Health (and ill health) is affected by the interplay between humans, animals and our shared environments. Research that takes these relationships into account benefits from the genetic, pathogenic and environmental diversity spanning the African continent.
Genetic diversity
Regarding genetic diversity, while it is commonly cited that Africa is one of the most diverse continents, the genome in Africa is actually still largely unmapped. However, a recently published whole genomic study reported great genetic diversity: After comparing the genetic variants from a relatively small sample of people from Africa to thousands of other African genomes in public databases, the researchers found three million novel genetic variants.2 Studies such as this, showing the extensive genetic variation among even geographically close African populations, highlight that there is not a single “representative” African population, and the study authors advocated for further characterization of genomic diversity of individuals in Africa in order to improve health.2
The findings of this study further support the argument that the genetic make-up of populations on the African continent is different enough from that of other populations that the indiscriminate use of genetic risk tools, such as polygenic scores, for health is not effective.3 Approximately two-thirds of studies developing risk scores are based on participants with European ancestry, 19% on participants of East Asian ancestry and only 4% of the studies included African, Hispanic or Indigenous populations.3 This limits our understanding of genetic predisposition to disease and the development of precision medicine for people of African descent.
A number of initiatives have been established to address this disparity, including the following:
Initiative
Location
Several countries in Africa (Nigeria, Ghana, Kenya and Ethiopia), United States and China
Entire African continent
Entire African continent
Key genetic findings include the protective effect of mutations in an LDL cholesterol pathway that are present in individuals with low LDL cholesterol levels of African descent but not in those of European descent.4 Another project investigates potential genetic reasons for the higher prevalence of rheumatic heart disease (RHD) in Black Africans than in other populations.5
These initiatives and findings impact decisions across the research spectrum. They allow us to better understand underlying genetic differences, how medicines might need to be tailored accordingly and potential differences in side effects and safety profiles that could affect pharmacovigilance plans. This is increasingly important as we move away from a one-size-fits-all approach to medicine and healthcare.
Demographic factors
There are also multiple changing demographic factors that could affect how and where research is conducted on the continent. For example, Africa is the world’s youngest continent, with 60% of the population younger than 25 years old6 and a median age of 20 years.7 It’s estimated that one-third of that age group globally will reside in sub-Saharan Africa by 2050.6
A lower-than-average life expectancy has contributed to the young population: across Africa, on average, men live to 63 years, and women live to 66 years (compared with global averages of 71 years and 75 years, respectively).8 However, with improvements in healthcare infrastructure and focused efforts to reduce the rates of high-priority infectious diseases such as HIV/AIDS, the situation is improving. It’s interesting to consider that continuing to align research with healthcare priorities could also move the life expectancy needle higher, improving individual as well as collective quality of life.
It’s interesting to consider that continuing to align research with healthcare priorities could also move the life expectancy needle higher, improving individual as well as collective quality of life.
Regarding living situation, use of land for urban development and the population living in urban areas are rapidly increasing.9 It’s estimated that by 2030, 17 cities in Africa will have more than five million inhabitants, and an additional 90 cities will have at least one million residents.6
What do these shifting demographics mean for health research?
- The younger generation is more tech-savvy than their older counterparts, and this could influence how and where research is conducted.
- Increasing life expectancy could influence which diseases are most prevalent and increase the incidence of non-communicable diseases that are common with older age.
- Movement of individuals from rural to urban areas could impact accessibility to healthcare services and research in some areas while also influencing disease characteristics such as transmissibility.
Pathogenic diversity
There’s also extensive pathogenic diversity, which has created challenges over the years in characterizing and identifying sources of disease, particularly during an outbreak. Many pathogens are also unique to the continent, reducing the ability to rely on pathogen genomic sequencing that has been conducted in other countries.
Yet, gaining a knowledge base of pathogens specific to diseases in Africa is of the utmost importance given the high burden of infectious disease outbreaks. In 2018, more than 140 disease outbreaks were reported, up from 123 in 2017.10 The reasons for the outbreaks were cholera (34 outbreaks in 19 countries), measles (16 countries), dengue fever (nine countries) and yellow fever (nine countries). In addition, there is a high incidence of microbial resistance.
With the aim of integrating pathogen genomics and bioinformatics into public health surveillance, outbreak investigations and disease control and prevention in Africa, the African Pathogen Genomics Initiative (APGI) was established.11 Part of the Institute of Pathogen Genomics launched by the Africa Centers for Disease Control and Prevention in 2019, the network will help inform research and public health responses to new epidemic threats such as COVID-19 as well as endemic diseases such as AIDS, tuberculosis, malaria and cholera. This expanded access to pathogenic sequencing in Africa can provide a more targeted response to current and emerging disease threats, including by sponsor-led research programs.
Environmental diversity
The multitude of pathogens is partly due to the varying environmental conditions in Africa, which range from arid deserts to savannas, tropical rain forests and extended highlands. The result is a broad biodiversity including ~60,000 known species of plants and ~123,000 known species of animals.12,13 At least 45,000 plant species (60% endemic) can be found in sub-Saharan Africa alone, which is the second-largest contributor to global plant diversity after South America.14
Yet again, there has been a lack of genomic sequencing to document Africa’s biodiversity. To date, little is understood about the broad animal, plant and marine ecosystems (and the effects of climate change and global movement) that contribute to both health and ill health. The African BioGenome Project (AfricaBP) is aiming to sequence the genomes of 105,000 endemic species: plants, animals, fungi, protists and other eukaryotes. Involving more than 100 African scientists and 22 African organizations, the store of reference genomes will broaden our understanding of the importance of endemic species, help build and sustain food systems for good nutrition and health, and contribute to drug development. In fact, it has been suggested that natural remedies could be investigated to treat leishmaniasis, a neglected disease without effective treatment options,15 as well as COVID-19.16 At the same time, it’s important to learn how natural remedies interact with registered medicines, both positively and negatively. In addition, novel structures from endemic natural sources might have a different mechanism of action that could help address resistance to commercial treatments.
Double disease burden: communicable and non-communicable diseases
The mix of factors detailed above is contributing to the continent’s disease profile. While the top three leading causes of death globally are non-communicable diseases (NCDs), namely heart disease, stroke and chronic obstructive pulmonary disease (COPD),17 in Africa, infectious diseases have long been top-leading causes of death. Infectious diseases represented three of the top five causes of death in Africa in 2019. However, non-communicable diseases such as ischemic heart disease and stroke are also climbing their way into the top rankings.
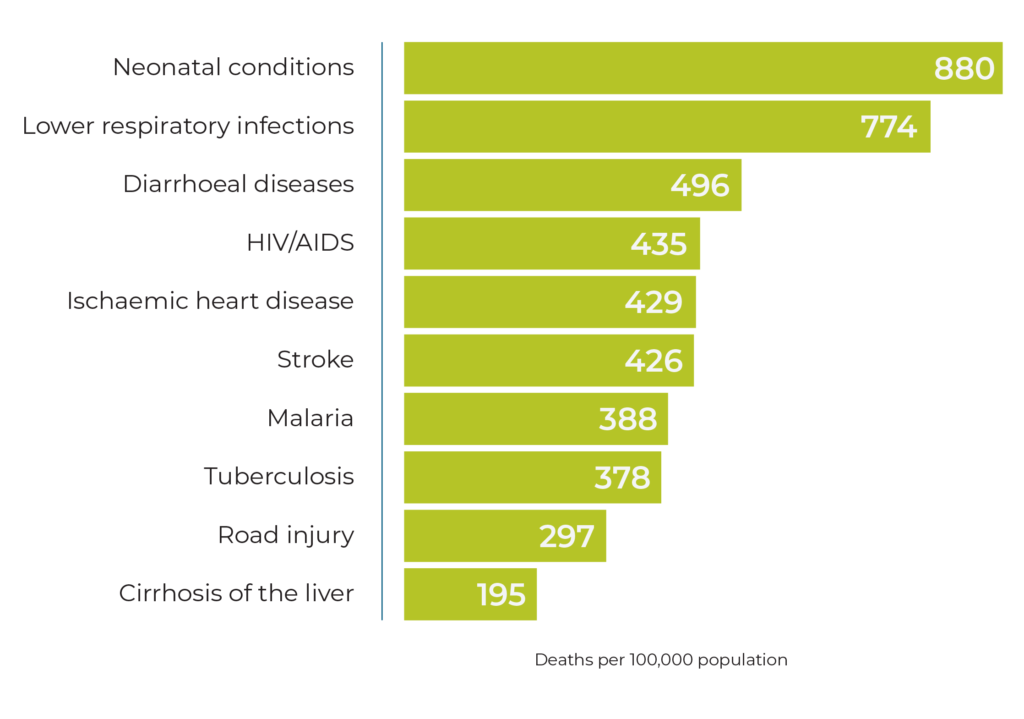
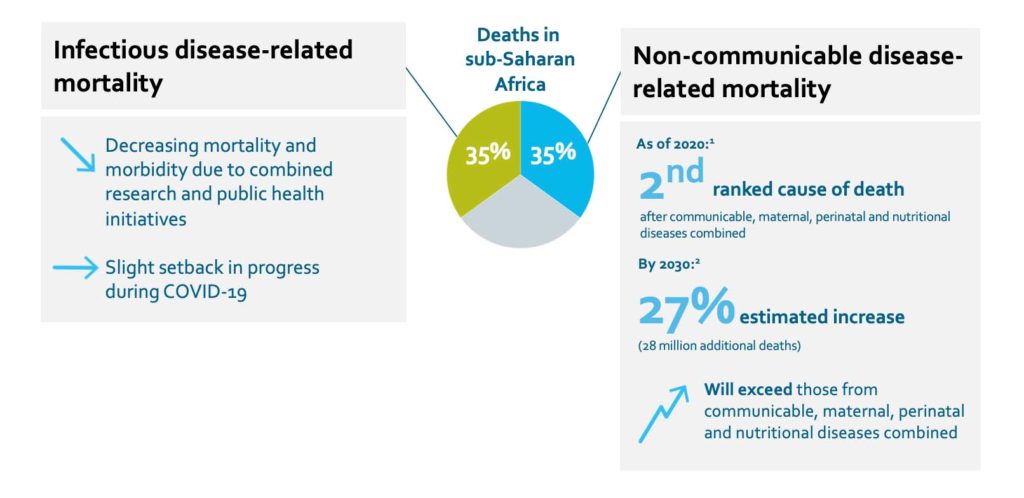
This has led to the current double disease burden across sub-Saharan Africa, with infectious diseases and NCDs contributing nearly equally to deaths.
Mortality and morbidity from infectious diseases has decreased due to targeted public health initiatives. For example, from 2005 to 2013, the prevalence of HIV/AIDS decreased from 5.6% to 4.7%, and AIDS-related deaths decreased by 40%, a period in which the Millennium Development Goals (MDGs) prioritized HIV/AIDS for healthcare investment and research in Africa.18 New cases of malaria, another MDG priority, decreased by 34% since 2000, while malaria-related deaths decreased by 54%. And average life expectancy increased by more than eight years, a greater increase than all other countries included in the MDG program.
However, some of this progress was stalled by the global shift in focus to COVID-19 research and pandemic-related disruptions to ongoing research for other infectious diseases. Many emerging and re-emerging diseases continue to cause outbreaks and are concerning for public health, including avian influenza, chikungunya, dengue fever, Ebola virus disease, hepatitis B virus, HIV, Lassa fever, malaria, Marburg virus disease, measles, meningitis, monkeypox and tuberculosis.
At the same time, the rates of NCDs are increasing at a rapid pace: 27% compared with a 17% increase globally. NCD-related deaths are estimated to exceed the number of deaths due to communicable, maternal, perinatal and nutritional diseases combined by 2030 in Africa.19 In sub-Saharan Africa, NCDs are the second-most common cause of death,20 and in some countries such as Mauritius, Namibia and Seychelles, NCDs cause between 50% and 88% of deaths.21 These increases have been attributed to poor infrastructure for NCD prevention and detection, as well as changing lifestyles.
Diabetes
Although the prevalence of diabetes in sub-Saharan Africa is relatively low, at 4.7% versus a global prevalence of 9.3%, this region is expected to have a 143% increase in prevalence by 2045.22 This figure is also likely under-reported since more than 60% of adults remain undiagnosed.23
Cardiovascular disease
Over the last three decades, there has been a 50% increase in CVD-related deaths in sub-Saharan Africa, many of which tend to occur at younger ages than in other areas of the world.24 Sub-Saharan Africa was the only geographical region globally with an increase in CVD-related deaths between 1990 and 2013.25
These values are likely under-reported, since, of adults with hypertension, more than 60% are undiagnosed and more than 75% are untreated.24
>60% of hypertensive adults are undiagnosed
>75% of hypertensive adults are untreated
It has been suggested that several sub-Saharan African countries are experiencing increasing prevalences of the traditional risk factors for CVD, including hypertension, obesity, diabetes mellitus and dyslipidemia.26
Oncology
An estimated 4% of the global total of new cancer cases in 2018 occurred in sub-Saharan Africa.27 The following top five cancers accounted for 50% of new cases in 2020: breast, cervix uteri, prostate, liver and colorectum. Although only 14% of the world’s female population resides in the region, more than one-third of all cervical cancer deaths globally occur in sub-Saharan Africa.
Intersection between communicable and non-communicable diseases
Communicable and non-communicable diseases don’t exist in isolation. There is evidence that each can contribute to mortality and morbidity of the other. For example, people with HIV have higher rates of CVD than those without HIV, potentially due to a combination of traditional CVD risk factors, HIV-related inflammation, highly active antiretroviral therapy (HAART) and opportunistic infections.24 Similarly, Africans with NCDs (especially hypertension, diabetes, CVD and asthma) are at higher risk of developing severe COVID-19.28 As the disease profile continues to encapsulate infectious diseases and non-communicable diseases, these interactions will continue to come to light, presenting both opportunities and challenges for research.
Africa: opportunities for clinical research
By excluding Africa from research programs in the past, we have missed out on potential solutions to public health issues that shorten lifespans; increase burden on the healthcare community, families and caregivers; and could inform research in other areas. Furthermore, as the “cradle of humankind,” the outcomes of research in Africa extend beyond the local communities to the global population. The research community should consider including sites and investigators in Africa to enrich its initiatives. We have further resources highlighting the potential of Africa as a research destination, including the recording of our webinar, Africa’s Potential for Clinical Research.
References
- Saleh M. Demographics of Africa – statistics & facts. Statista, May 9, 2022. Available at: https://www.statista.com/topics/7928/demographics-of-africa/
- Choudhury A, Aron S, Botigué LR, et al. High-depth African genomes inform human migration and health. Nature 2020;586:741–748. https://doi.org/10.1038/s41586-020-2859-7
-
Duncan L, Shen H, Gelaye B, et al. Analysis of polygenic risk score usage and performance in diverse human populations. Nat Commun 2019;10(3328).
https://doi.org/10.1038/s41467-019-11112-0 - Cohen J, Pertsemlidis A, Kotowski IK, et al. Low LDL cholesterol in individuals of African descent resulting from frequent nonsense mutations in PCSK9. Nat Genet 2005;37:161-165. https://doi.org/10.1038/ng1509
- Machipisa T, Chong M, Muhamed B, et al. Association of Novel Locus With Rheumatic Heart Disease in Black African Individuals: Findings From the RHDGen Study. JAMA Cardiol 2021;6(9):1000-1011. doi:10.1001/jamacardio.2021.1627
- Dews F. Charts of the Week: Africa’s changing demographics. Brookings, January 18, 2019. Available at:
https://www.brookings.edu/blog/brookings-now/2019/01/18/charts-of-the-week-africas-changing-demographics/ - Saleh M. Population of Africa in 2021, by age group. Statista, July 15, 2022. Available at: https://www.statista.com/statistics/1226211/population-of-africa-by-age-group/
- Kamer L. Life expectancy in Africa 2021. Statista, February 1, 2022. Available at: https://www.statista.com/statistics/274511/life-expectancy-in-africa/
- Jiang S, Zhang Z, Ren H, et al. Spatiotemporal Characteristics of Urban Land Expansion and Population Growth in Africa from 2001 to 2019: Evidence from Population Density Data. ISPRS Int. J. Geo-Inf. 2021, 10(9), 584; https://doi.org/10.3390/ijgi10090584
- World Health Organization. Regional Office for Africa. (2020). Emergency Operations Annual Report: saving lives and reducing suffering WHO’s work in emergency response operations in the WHO African Region in 2018. World Health Organization. Regional Office for Africa. Available at: https://apps.who.int/iris/handle/10665/330396
- Makoni M, Africa’s $100-million Pathogen Genomics Initiative. The Lancet: Microbe. 2020;1(8):E318. https://doi.org/10.1016/S2666-5247(20)30206-8
- Ebenezer TE, Muigai AWT, Nouala S, et al. Africa: sequence 100,000 species to safeguard biodiversity. Nature 2022.
- Marks RA, Hotaling S, Frandsen PB, et al. Representation and participation across 20 years of plant genome sequencing. Nat. Plants 2021;7:1571-1578.
https://doi.org/10.1038/s41477-021-01031-8 - Linder HP. The evolution of African plant diversity. Front Ecol Evol 2014. https://doi.org/10.3389/fevo.2014.00038
- Surur AS, Fekadu A, Makonnen E, et al. Challenges and Opportunities for Drug Discovery in Developing Countries: The Example of Cutaneous Leishmaniasis. ACS Med Chem Lett 2020;11(11):2058-2062. doi: 10.1021/acsmedchemlett.0c00446.
- Francis AA, Adebayo FA, Olujide O, et al. Therapeutic Potentials of Antiviral Plants Used in Traditional African Medicine With COVID-19 in Focus: A Nigerian Perspective. Frontiers in Pharmacology 2021;12. https://www.frontiersin.org/articles/10.3389/fphar.2021.596855
- Percentage of leading 10 causes of death worldwide in 2019. Statista. Available at:
https://www.statista.com/statistics/311925/top-ten-causes-of-death-worldwide/ - Narayan K, Donnenfeld Z. Envisioning a healthy future: Africa’s shifting burden of disease. Institute of Security Studies. 2016. Available at:
https://korbel.du.edu/sites/default/files/2021-12/Envisioning%20a%20Healthy%20Future.pdf - Dicker D, Nguyen G, Abate D, et al. Global, regional, and national age-sex-specific mortality and life expectancy, 1950–2017: a systematic analysis for the global burden of disease study 2017. Lancet 2018;392(10159):1684-1735.
- A systematic analysis for the Global Burden of Disease Study 2017. Default results are deaths and DALYs for 2017 with trends since 1990. 2017. Available at:
http://ghdx.healthdata.org/gbd-results-tool - Deaths from noncommunicable diseases on the rise in Africa. World Health Organization. April 11, 2022. Available at:
https://www.afro.who.int/news/deaths-noncommunicable-diseases-rise-africa
https://doi.org/10.1016/j.diabres.2019.107843 - Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Research and Clinical Practice 2019;157:107843.
- Africa: Diabetes report 2000-2045. International Diabetes Federation. Available at: https://diabetesatlas.org/data/en/region/2/afr.html
- Yuyun MF, Sliwa K, Kengne AP, et al. Cardiovascular Diseases in Sub-Saharan Africa Compared to High-Income Countries: An Epidemiological Perspective. Glob Heart 2020;15(1):15. doi: 10.5334/gh.403
- Roth GA, Forouzanfar MH, Moran AE, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med 2015;372:1333-1341. doi: 10.1056/NEJMoa1406656
- Amegah AK. Tackling the Growing Burden of Cardiovascular Diseases in Sub-Saharan Africa. Circulation 2018;138:2449-2451.
https://doi.org/10.1161/CIRCULATIONAHA.118.037367 - Sub-Saharan Africa. The Cancer Atlas. Available at:
https://canceratlas.cancer.org/the-burden/sub-saharan-africa/ - Noncommunicable diseases increase risk of dying from COVID-19 in Africa. World Health Organization Regional Office for Africa. September 10, 2020. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7470795/